Profylax med antibiotika mot infektion i kirurgin
advertisement

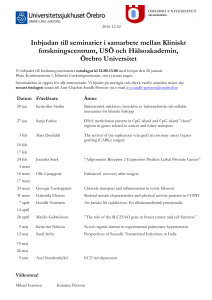
Profylax med antibiotika mot infektion i kirurgin Per-Olof Nyström Gastrocentrum kirurgi Karolinska Antibiotikaförsäljning, slutenvård i Sverige under perioden 2001 - 2007. Sverige Stockholm DDD per 650 1000 inv. 600 550 500 450 400 350 300 2001 2002 2003 2004 2005 2006 2007 GCK Karolinska Antibiotika Kostnader 2011 1 Antifungala medel 2 1603921 70,5% Carbapenem, Pip-Tazo 317363 14% 3 Vankomycin, Zyvoxid 101053 4% 4 Kinoloner 53484 5 Cefalosporiner 43868 6 Tetracyklin, Tigecyklin 35051 7 Erytromycin m fl 31066 8 Aminoglykosider 19465 9 Penicillinas stabila 18952 10 Penicilliner 18686 11 Antivirala medel 17085 Totalt 2259994 99% Duration of intravenous antibiotic treatment in 29 patients with postoperative complication (n=25) or primary infection (n=4) 29/141 = 20.6 percent 20 18 16 Mean 7.2 days, median 6 days. Antal dagar 14 12 10 8 6 4 2 0 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 Patient NAK (H) Sep 2009 – Mar 2010 Indications for intravenous antibiotic treatment in 29 patients with postoperative complication (n=25) or primary infection (n=4) Primary infection or extended prophylaxis 4 Anastomotic leakage 6 Abscess 5 Wound healing problems 5 SIRS 4 Pneumonia or respiratory problem 3 Peritonitis 2 6/29 had follow-up treatment with oral antibiotics K73 Data Sept 2009 to March 2010 Trauma Infektion SIRS Brännskada Pankreatit Akut kolit Postoperativ Systemic inflammatory response syndrome Cancer Bone et al. Chest 1992 Explanation models for surgical infection Hygiene Hygiene Surgery Surgery Physiology Physiology National Inpatient Sample database (US) for elective colon resection and cholecystectomy Davis et al. SIS annual meeting 2011 The Surgical Care Improvement Project, SICP, does not prevent surgical site infection in colorectal surgery. Period A n=238 Period B n=258 SSI rate 19 % 19 % Superficial 12 % 13 % Deep wound 2 % 0.5 % Organ space 5 % 5 % Pastor et al. DCR2010;53:24-30 Surgical Site Infection Incision Organ space Over all Laproscopy 12,3 7,5 19,8 Open 13,2 12,1 25,3 605 colorectal procedures requiring a resection and anastomosis. Operated between 2001 – 2008 at NY Presbytarian Hospital. 94 % Clean-contaminated, 71 % ASA II, mean Age 60 years. Ho et al. Surgical Infections 2011;12:255-60. Duration of intravenous antibiotic treatment in 29 patients with postoperative complication (n=25) or primary infection (n=4) 29/141 = 20.6 percent 20 18 16 Mean 7.2 days, median 6 days. Antal dagar 14 12 10 8 6 4 2 0 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 Patient NAK (H) Sep 2009 – Mar 2010 Medicare database 2005 & 2006, (269 911 patients); Incidence of complication Best 0 2 4 6 Worst 8 10 12 14 % Respiratory Pneumonia MI DVT/PE Renal GI bleed Haemorrhage SSI Ghaferi et al. Ann Surg 2009;250:December How common is SWI in colorectal surgery ? Test arm No. of 24 trials 22 Control arm No. of 24 trials 22 Median 9.9% IQR 9.7 20 20 18 18 16 16 14 14 12 12 10 10 8 8 6 6 4 4 2 2 0 0 0 5 10 15 20 Percent SWI After Song et al. BJS 1998 25 30 Median 9.7% IQR 8.9 35 40 0 5 10 15 20 Percent SWI 25 30 35 40 Sir (Arnold) Ashley Miles (1904-1988) Professor of Experimental Pathology Director, Lister Institute of Preventive Medicine in London John F. Burke Hiram C. Polk Harvard, Boston Louisville, Kentucky Mechanism of Antibiotic prophylaxis 1961 Första randomiserade profylaxstudien 1969 Miles, Miles, Burke. The value and duration of defence reactions of the skin to the primary lodgement of bacteria. Br J Exp pathol 1957;38:79-96. Burke. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery 1961;50:161-8. Polk, Lopez-Mayor. Postoperative wound infection: a prospective study of the determinant factors and prevention. Surgery 1969;66:97-103. PowerPoint stoppade automatisk hämtning av den här bilden för att sk y dda din integritet. The Epidemiology and Other Problems of Wound Infection Sir Arthur Ashley Miles University of Cambridge 1952 0 1 2 3 4 timmar 12 mm 10 8 6 4 2 mm 105 avdödade eller levande S.aureus Decisive period = Effective period ≈ 4 tim 8 E. coli B. fragilis 7 Log. Conc. per ml 6 5 4 3 2 1 0 4 8 12 Hours 16 20 24 Pure bacterial contamination Bacterial/faecal contamination 9 8 E. coli E. coli b1 B. fragilis 7 B. fragilis 6 Log. Conc. per ml Log. Conc. per ml 8 5 4 3 7 b2 6 2 a2 a1 5 1 0 4 8 12 16 Hours 20 24 0 4 8 12 Hours 16 20 60 Surgical 50 Wound Infection 40 (%) wet wound placebo, wound Hct > 8% dry wound placebo 30 20 10 dry wound with antibiotic 0 0 1 2 3 4 5 6 Log wound bacteria After Polk & Lopez Mayor 1969 Kirurgiska infektionens patogenes (kortformen) Hematomet är den kirurgiska infektionens kuvös. Antibiotika i hematomet är profylaxens mekanism. Varje sår med läkningsstörning blir sekundärt infekterat American Society of Health-System Pharmacists Therapeutic Guidelines for Antimicrobial Prophylaxis in Surgery Cardiothoracic Cefazolin Gastrointestinal Cefazolin Biliary Cefazolin Colorectal Neomycin+Erytromycin base or Cefoxitin Head & neck Cefazolin Craniotomy Cefazolin Obstetric, Gyn Cefazolin Orthopedic Cefazolin Vascular Cephazolin Urology Sulphamethoxazole Transplant Cefazolin Cefazolin: Eli Lilly 1964 Am J Health-Syst Pharm. 1999; 56:1839–88. Timing of antibiotic prophylaxis Type of surgery Number of cases Optimal time Clean‐contaminated 2847 Within 2 hrs Elective 9195 1 or 2 hrs Colorectal 3836 30 – 60 min Colorectal 605 30 min Classen et al. NEJM 1992;326:281-86. Hawn et al. JACS 2006:203:803-11. Weber et al. Ann Surg 2008;247:918-26. Steinberg et al. Ann Surg 2009;250:10-16. Ho et al. Surgical Infections 2011;12:255-60. Två inställningar: 1. Ab profylax skall bara ges till kirurgi med bevisad effekt på infektioner? 2. Ab profylax är en generell behandlingsprincip i kirurgin. Is Antibiotic Prophylaxis in Surgery a Generally Effective Intervention? Meta-analyses published between1990 and 2006 of randomized controlled trials that looked at the effectiveness of prophylactic antibiotics versus no antibiotic or placebo The hypotheses to be assessed were: 1. antibiotic prophylaxis is an effective intervention for preventing wound infection over a broad range of different surgical procedures, 2. there is a substantial difference in the effectiveness of antibiotic prophylaxis between “clean” and “contaminated” surgical procedures. Bowater et al. Ann Surgery 2009;249:551 The hypotheses to be assessed were: 1. antibiotic prophylaxis is an effective intervention for preventing wound infection over a broad range of different surgical procedures: 2. there is a substantial difference in the effectiveness of antibiotic prophylaxis between “clean” and “contaminated” surgical procedures. Hypothesis #1: Effectiveness over 23 types of surgery was significant and similar, all RR <1. Hypothesis #2: No evidence of a difference with wound class. Bowater et al. Ann Surgery 2009;249:551 Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. Cochrane Database of Systematic Reviews 2010, Issue 3. William J Gillespie & Geert HIM Walenkamp Review included 23 trials, involving a total of 8447 participants. Reduced incidence of deep infection: risk ratio 0.40, 95% CI 0.24 to 0.67 No added benefit of multiple dosing. Economic modelling using data from one large trial indicated that single dose prophylaxis with ceftriaxone is a cost-effective intervention. Meta-analysis of the effectiveness of prophylactic antibiotics in the prevention of postoperative complications after tension-free hernioplasty. Included 6 studies with 2235 patients Infection rate 1,7 % vs 3,8 % OR 0.45 (95% CI 0.26–0.77, p = 0.004), number needed to treat 48 (cefazolin, cefuroxime, amoxicillin-clavulanic acid) Jian-Fang Li et al. (China) Can J Surg, 2012;55:27-32 Systematic review and meta-analysis of the effectiveness of antibiotic prophylaxis in prevention of wound infection after mesh repair of abdominal wall hernia Six studies of 2507 patients with femoral or inguinal hernia. Infection rate 1,5 % versus 3,0 %. odds ratio 0·54, 95 per cent CI 0·24 to 1·21 Number needed to treat was 74. (cefazolin, cefuroxime, amoxicillin-clavulanic acid) Aufenacker et al. BJS 2006; 93: 5–10 Systematic review of Ab prophylaxis in colorectal surgery Favouring intervention +5 % 0 Favouring control -5 % 1968 1970 1980 year Baum et al. NEJM 1981;305:795-9 Surgical Wound Infection in colorectal surgery ? Test arm No. of 24 trials 22 Control arm No. of 24 trials 22 Median 9.9% IQR 9.7 20 20 18 18 16 16 14 14 12 12 10 10 8 8 6 6 4 4 2 2 0 0 0 5 10 15 20 Percent SWI After Song et al. BJS 1998 25 30 Median 9.7% IQR 8.9 35 40 0 5 10 15 20 Percent SWI 25 30 35 40 Antimicrobial prophylaxis for colorectal surgery. Nelson, Glenny & Song: Cochrane Systematic reviews 2009. 161 studies. Ab prophylaxis vs. none RR 0.3 Single dose vs. multiple dose RR 1.06 Additional anaerobic coverage RR 0.55 Additional aerobic coverage RR 0.41 Different antibiotics vs. Gold standard RR 0 (no difference) Antibiotic Prophylaxis in Obstetric Procedures 1. All women undergoing elective or emergency Caesarean section should receive antibiotic prophylaxis. (I-A) 2. The choice of antibiotic for Caesarean section should be a single dose of a first-generation cephalosporin. (I-A) 3. The timing of prophylactic antibiotics for Caesarean section should be 15 to 60 minutes prior to skin incision. (I-A) 4. If an open abdominal procedure is lengthy (> 3 hours) or estimated blood loss is greater than 1500 mL, an additional dose of the prophylactic antibiotic may be given 3 to 4 hours after the initial dose. (III-L) 5. Prophylactic antibiotics may be considered for the reduction of infectious morbidity associated with repair of third and fourth degree perineal injury. (I-B) Van Schalkwyk & Van Eyk JOGC September 2010 Gastrocentrums kirurgi Ab-program Oral profylax för planerad kirurgi: T. Bactrim forte eller Eusaprim forte 1 tabl. T. Flagyl 3 tabl. à 400 mg = 1,2 g Vid känd sulfa allergi kan Bactrim ersättas med T. Doxyferm 4 tabl Antibiotika profylax i kirurgins praktik 1. Profylax är för elektiv patient utan aktuell infektion. 2. Single-dos som regel. 3. Kan upprepas vid lång operation > 4 tim. 4. Ingen profylaxdos efter avslutad op. 5. Intravenös dos 30 min före incision. 6. Oral dos 1 tim före incision. 7. Effekten är ca halvering av infektionerna. 8. Många olika antibiotika fungerar, välj något som inte används för terapi. Antibiotikaprofylaxen är ett endimensionellt sätt att se på den kirurgiska infektionen. Riskfaktorerna är många hos patienten. Läkningsstörningar är vanliga. Stor kirurgi och komplex kirurgi dubblar komplikationerna.